Optimizing Outcomes and Controlling Cost through Proactive Discharge Planning
THE VALUE OF A GOOD HOSPITAL DISCHARGE PLANNING PROGRAM, SOMETIMES REFERRED TO AS TRANSITIONS OF CARE COORDINATION, IS VITAL.
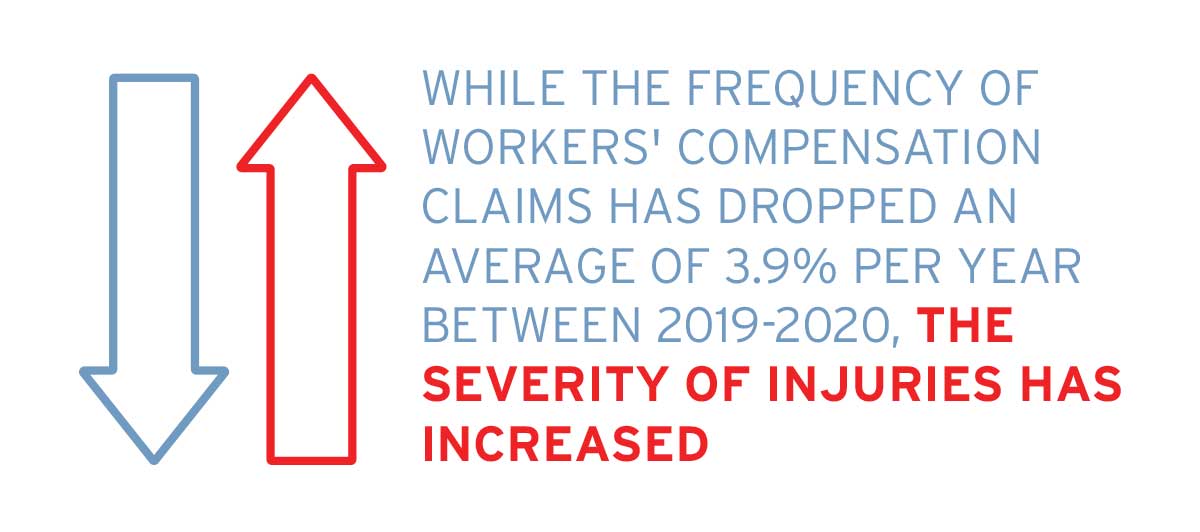
A discharge planning program has the ability to help reach an optimal health outcome for the injured worker, as well as help with cost savings for the insured. Data shows that, while the frequency of workers’ compensation claims has dropped an average of 3.9% per year between 2019-2020, the severity of injuries has increased (1). This is largely due to an aging workforce, as well as the compromised baseline health of injured workers resulting from comorbidities such as diabetes, metabolic syndrome, and cardiovascular disease. For example, an injury previously resulting in a knee or shoulder repair may now require a replacement which results in higher acuity and thus higher potential for complications postop.


After a hospital stay, nearly 20% of injured workers will experience an adverse event within 30 days of discharge, many of which could have been avoided (2). A great deal of these complications can be attributed to poor discharge planning. Factors in these complications could be medication changes or discrepancies or ineffective education for family members to be aware of danger signs. Failure to confirm clinician teaching and injured worker understanding, and lastly a discontinuity between the inpatient and outpatient providers (2).
The primary role of the case manager is to facilitate communication between all members of the interdisciplinary team resulting in optimal outcomes for the injured worker and overall cost savings. Once the need for surgery has been determined, it is worthwhile to consider assigning a case manager to help assist with the discharge planning process. Proactive discharge planning is a critical component to optimizing health outcomes for the injured worker and controlling costs for the insured. While there will always be injuries resulting in surgeries, outcomes and cost can be greatly impacted through a case management commitment to proactive discharge planning. Employing case management as an early intervention strategy ensures optimal recovery for the injured worker and guarantees cost savings for the account. Cost savings are greatly maximized when case management needs are identified early in the process.
THE PHASES OF DISCHARGE PLANNING: FAMILY ENGAGEMENT
Case managers understand the discharge planning process starts well before any admission to the hospital. To a large degree, the case manager’s preparedness in the pre-op period sets the stage for the entire rehabilitation process. Securing a successful rehabilitation for an injured worker starts with effective engagement of his/her family and involving them as part of the rehabilitation team. Research shows that when the family is engaged in the discharge process and rehabilitation plan, quality improves, and there is a reduction in preventable readmissions (2). Empowering the injured worker and their family members helps to share in the responsibilities of the rehabilitation plan and changes the overall atmosphere of the recovery process along with the return-to-work efforts.
Key elements of discharge planning include engaging with family members as members or associates of the interdisciplinary care team. Family education on what to expect upon discharge can help prepare them mentally as well as logistically for this phase of the rehabilitation. The case manager can describe what life at home will be like post-op for the injured worker and their family. Reviewing all medications, including their actions and potential side effects, can help prevent unnecessary medication errors such as contraindications between medications and common warning signs or problems.
Reviewing the post-op discharge instructions with the family members helps them to understand what is expected of them after they leave the hospital. When using education and guidelines-based clinical management compared to standard primary care, it has been found that combining these interventions improves short- and long-term work disability outcomes and are cost-effective. By involving family members with the injured worker’s recovery, fewer workers require longterm disability compensation and lost-work episodes were shorter.
Assisting the family with the coordination of post-op appointments with all members of the care team should be done sooner rather than later. Asking the family members pointed questions on next steps etc., to help gauge their level of understanding is an important facet of the case management process and provides the opportunity for re-education when needed which can alter outcomes. It also provides the case manager with insight into the family’s preferences, goals, and concerns, which will better prepare the case manager to tailor his/her interventions with the family to better suit their immediate needs.


PRE-OP PREPAREDNESS
In the pre-op period, the case manager is also responsible for ensuring all medical authorizations are received, all pre-op testing is completed with necessary medical clearance provided to the surgeon’s office. All post-op DME and medications and services are approved and coordinated for the immediate post-op period. These essential pre-op steps are all facets of the discharge planning process, which demonstrates that the discharge planning process starts before the hospital admission of the injured worker.
For example, by aligning medical clearance processes the case manager can minimize cancellations and increase efficiency. In regard to obtaining medical clearance and preop testing, some injured workers may require only routine pre-admission testing such as a physical exam and an EKG, while others will require a more focused medical clearance or release from their cardiologist or specialist. Additionally, coordination of necessary post-op medications and DME, such as anticoagulant therapy and ambulatory devices, like a knee scooter or crutches, are essential to optimal outcomes for the injured worker. Furthermore, the case manager will ensure that all pre/ post-op lab testing, such as PT/PTT or INR testing, will be performed if the injured worker is on anticoagulants or has a pre-existing liver or bleeding disorder. Early identification of risk factors and mitigation of complications via preparedness such as medication coordination, DME, and labs greatly impacts the rehabilitation for the injured worker and subsequent cost for the insured.
- Anticipated discharge date
- Medical records sent to receiving facility or to outpatient providers
- Name and contact number of the agency performing the service of home health, skilled nursing visits, or home physical or occupational therapy
- Simple instructions such as post-op wound care steps and bandage change schedules
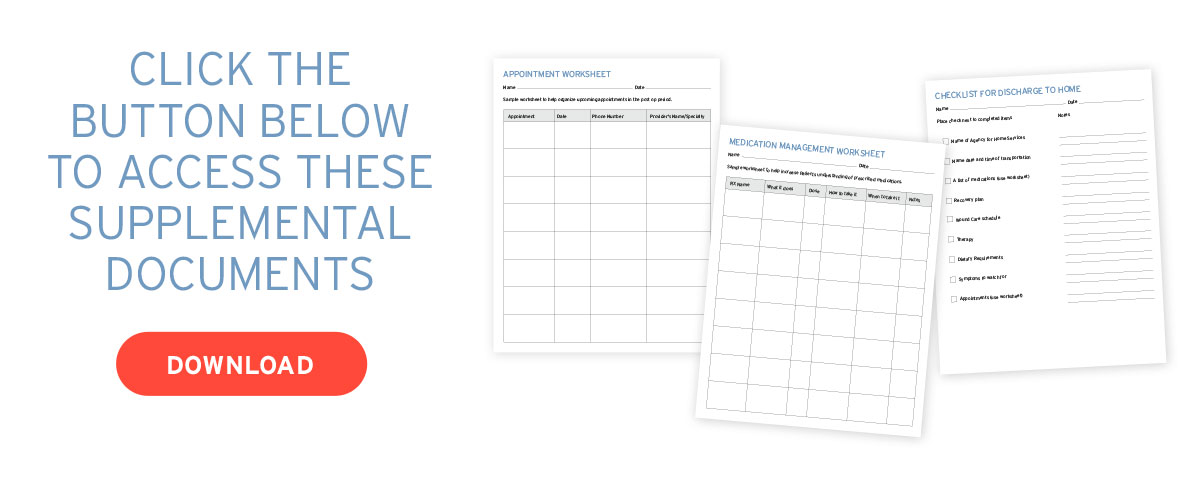
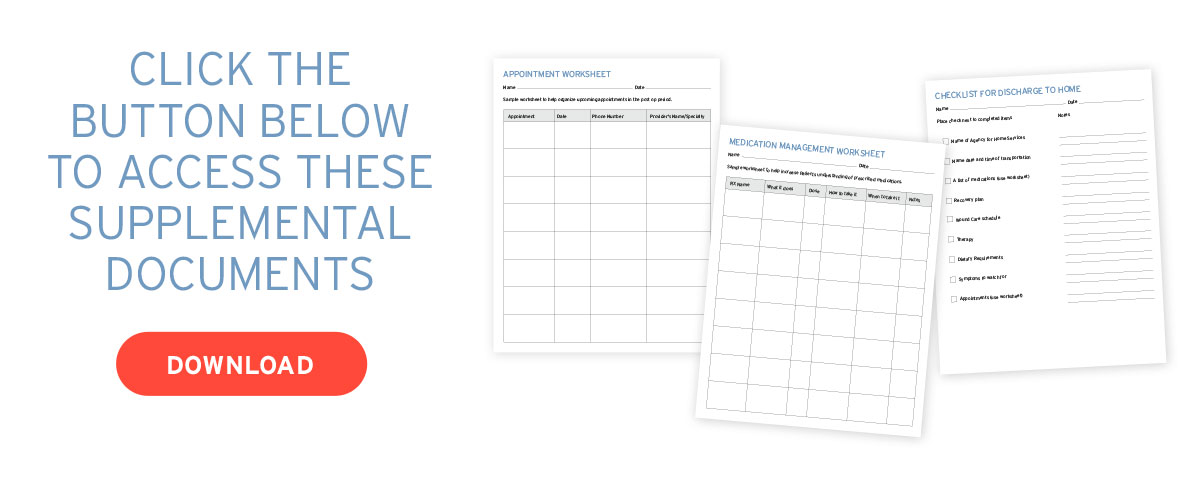
- An appointment worksheet to help remind the injured worker of appointments that may already be scheduled or that require scheduling, as well as the name and specialty of the provider
- A medication management worksheet to remind the injured worker of his/her lists of medications with dose and frequency, a list of symptoms to watch out for, and when to seek medical care (3).
THE POST-OP PERIOD
The case manager’s role is to assist with coordination of care and transfer of care for the injured worker from the hospital to home or post-acute setting. After transfer, the case manager facilitates communication regarding the injured worker’s recovery to the adjuster, employer, and attorney team. Case managers also help coordinate follow-up appointments, all therapy visits, any necessary transportation, as well as to help monitor any follow-up care with the clinical team and Primary Care Providers.


The reality of today’s fast-paced healthcare system can be overwhelming for the injured worker to navigate. The added value of having a point person, such as the case manager, who can facilitate communication to all team members and help to ensure all necessary pre- and post-op steps are completed, is key to ensuring an optimal outcome. Lastly, the importance of timely communication on the post-op status for the injured worker, who was discharged to a post-acute setting, is critical to minimizing an injured worker’s length of stay at the post-acute setting and provides substantial cost savings.
HOME CARE
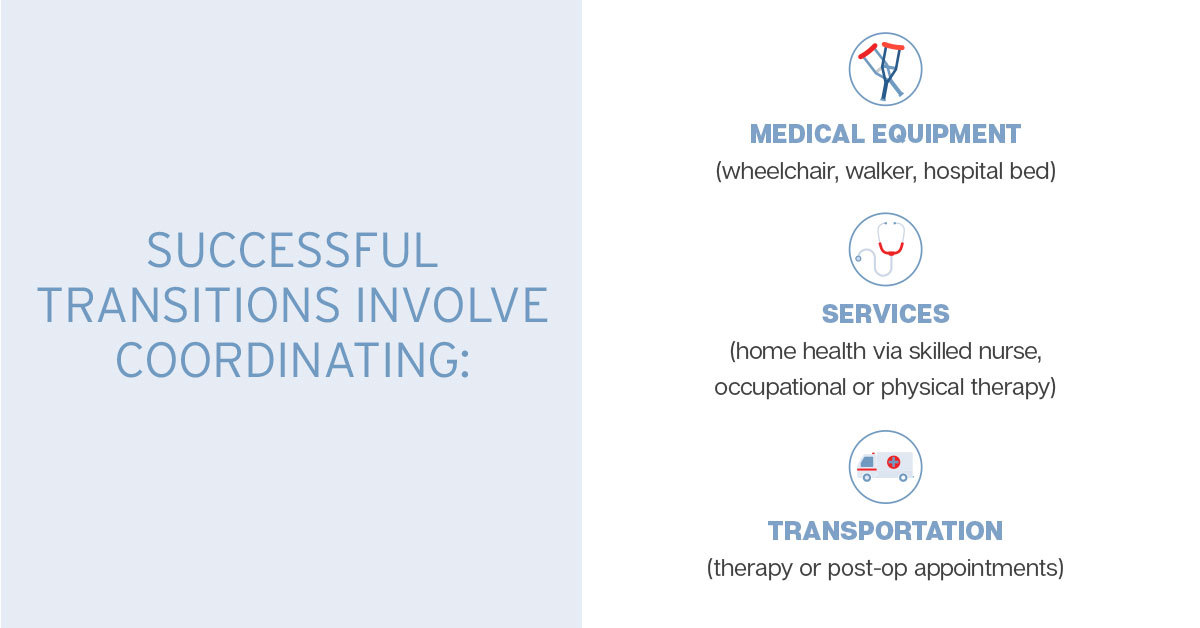
The injured worker’s discharge from the hospital to home will require a certain amount of coordination to make the transition home successful. After being discharged from the hospital, many injured workers will require ongoing services in their rehabilitation. The case manager will coordinate any medical equipment needed by the injured worker, such as a wheelchair, walker, or hospital bed. The case manager will also coordinate services such as home health via a skilled nurse, occupational or physical therapy. The case manager will also coordinate transportation to therapy or post-op appointments with their doctors. The importance of helping the family prepare for an injured worker’s return home can be something as simple as considering stairs to and from the bedroom or sleeping considerations such as a recliner for a temporary period post-op. These simple steps can help assist the injured worker in achieving the necessary post-op rest, which can result in better outcomes.
SUCCESS STORY
Post Spinal Fusion DISCHARGE PLANNING – DEC 2021
A request was received to assist with the discharge planning of an injured worker (IW) with a post-op spinal fusion. The IW is a 49-year-old male who was 1-week S/P lumbar fusion. This was the second surgery for this same back issue in three months, as the degree of repair involved both the anterior and posterior approach, necessitating two separate surgeries. This request was received nine days before Christmas 2021. The IW resided in Michigan. The case manager contacted the facility and worked directly with the onsite social worker discharge planner who was responsible for the IW while in-house at the hospital. The case manager made her introductions to the hospital team and requested all updated medical records, reports, and orders for discharge, including discharge instructions. The case manager reached out to the IW and his wife to introduce herself and explained her role. The IW and his family were greatly relieved to have someone to assist with the coordination of all the post-op orders, as they reported feeling overwhelmed, especially with the holidays fast approaching.
The case manager worked with the hospital discharge planner and the claims examiner to price out Home Health Services that was ordered for this IW. The home health services would include Skilled Nursing Visits (SNV), as well as OT and PT. Emphasizing the importance of continuity of care, the case manager was able to obtain approval for the post-op home health services that were affiliated with the hospital where he underwent his surgery and also where his providers were based. Carlisle Medical was able to facilitate his post-op prescriptions through the PBM and ensure prompt delivery of all medications to his home. Carlisle coordinated all the post-op DME through our own DME department, which arrived on time and without issue. The case manager maintained daily contact with the home health agency, as well with the IW and family, providing timely updates to the account on the IW’s progress and status post-op. Once all services were in place, the case manager assisted the IW with the coordination of his post-op appointments and attended the first few visits to ensure a soft transfer from home health services to outpatient formal PT. The account and the family were very appreciative of our efforts, especially at such a challenging time before the holidays.
REFERENCES
[1] Coate, Patrick. Changing Workforce Demographics and Workplace Injury Frequency. Retrieved November 11, 2022, from http://www.ncci.com/Articles/Documents/Insights-WorkforceDemographics.pdf
[2] Foster AJ, Murff HJ, Peterson JF, et al. The incidence and severity of adverse events affecting injured workers after discharge from the hospital. Ann Intern Med. 2003; 138(3):161-7.
[3] Checklist for Discharge to Home. Retrieved November 11, 2022, from https://www.nurseregistry.com/wp-content/uploads/hospital-discharge.pdf
ADDITIONAL RESOURCES
This white paper was prepared by Jeff Carlisle, Vice President for Carlisle Medical, in collaboration with staff and pharmacists. Carlisle Medical has more than 35 years of experience as a leader in health care cost containment in the workers’ compensation industry. Our company assists insurance carriers, third-party administrators, and employers significantly reduce their workers’ compensation costs. Our experienced staff of licensed pharmacists and nurses can assist companies with injuries ranging from minor to catastrophic.