Fighting the War On Opioids in the Workers’ Compensation Industry
THE PREVALENCE OF OPIOID USE AND ABUSE AMONG THOSE WITH CHRONIC PAIN HAS DEVELOPED INTO ONE OF THE MOST PRESSING ISSUES TODAY. THIS ISSUE, COMMONLY REFERRED TO AS THE OPIOID CRISIS, SPANS MANY DISCIPLINES IN THE HEALTHCARE INDUSTRY AND IS GAINING WIDESPREAD ATTENTION AS IT CLAIMS THOUSANDS OF LIVES EACH YEAR.


In 2016, more lives were lost in the United States to opioid related drug overdoses (42,294) than to motor vehicle accidents (37,461).[1] Anne Schuchat, M.D., acting director of the Centers for Disease Control and Prevention (CDC), stated, “The amount of opioids prescribed in the U.S. is still too high, with too many opioid prescriptions for too many days at too high a dosage. Health care providers have an important role in offering safer and more effective pain management while reducing risks of opioid addiction and overdose.”[2] The overuse of prescription opioids varies between regions of the United States.
For example, recent findings indicate opioids such as Norco® are the most commonly prescribed medication in 10 states, including Alaska, Alabama, Georgia, Idaho, Illinois, Indiana, Mississippi, North Carolina, Nebraska, and Oklahoma.[3] According to the latest CDC report, 40 percent of the more than 40,000 overdose deaths that occurred in 2016 were linked to prescription opioids.[4] This exceeds all historical data reported.
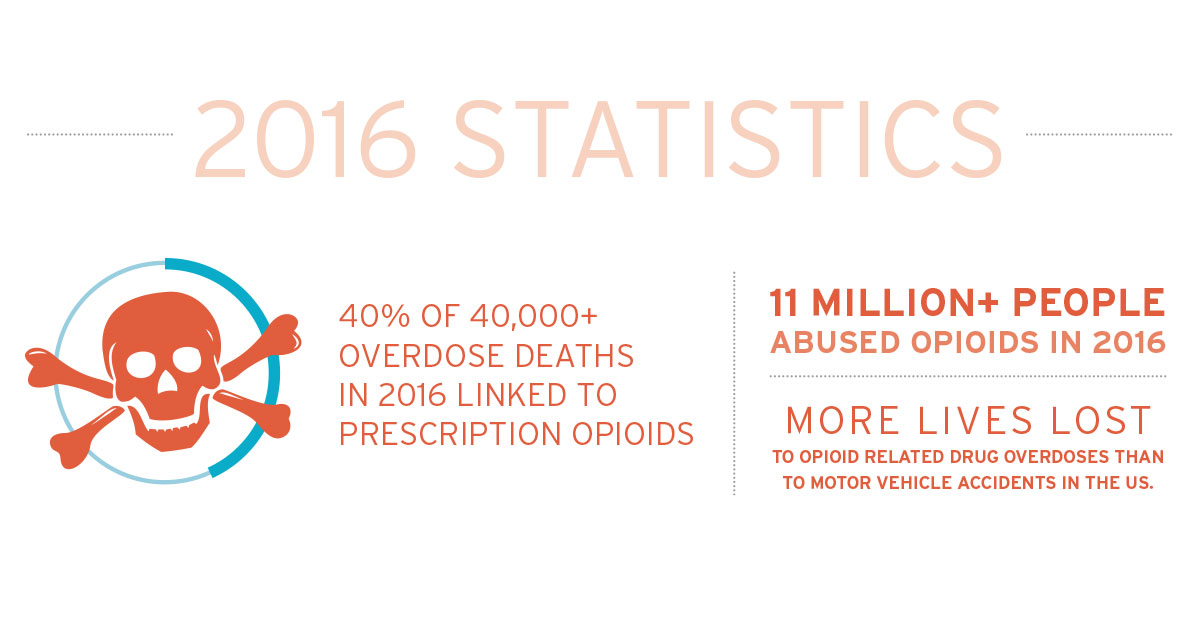
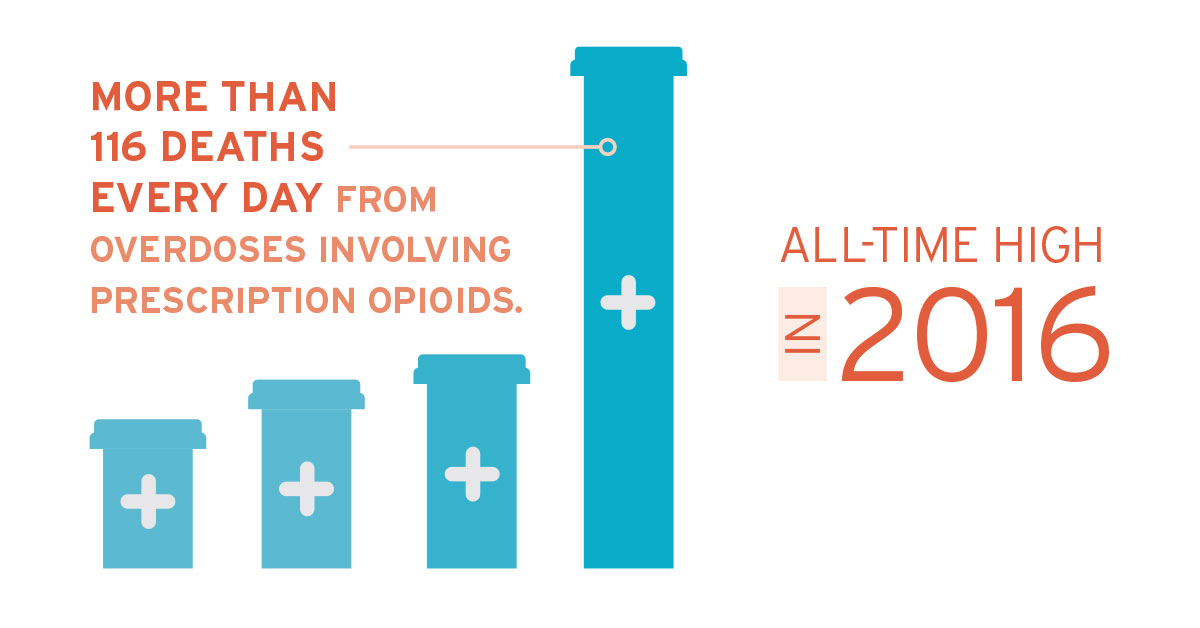
Opioids continue to be the main driver of drug overdose deaths. In fact, opioid overdose deaths were five times higher in 2016 than 1999—further demonstrating a 16-year rise in overdose deaths involving prescription opioid pain relievers.[5]
This issue has garnered more interest in recent years from the American people and public officials. In 2016, President Barack Obama called for $1.1 billion in funds to address the opioid crisis.[6] More recently, in 2017, President Donald Trump declared the opioid epidemic a “national emergency.” The increase in public awareness bodes well for payers in the workers’ compensation industry who may benefit from these new initiatives.
Over the last 10 years, states and research institutes in the workers’ compensation industry have been working extensively to control the use of opioids. Pharmacy Benefit Managers (PBM) continue to conduct their own research and utilize industry research to develop programs that identify and implement safer and more cost-effective alternatives.
WHAT IS AN OPIOID?
An opioid is a specific type of narcotic pain medication that is used to treat moderate to severe pain. Opioids are natural or synthetic chemicals that interact with opioid receptors in the brain to reduce the intensity of pain signals and the feeling of pain. Opioids are available in numerous forms–tablets, capsules, skin patches, liquid form for oral use and injection, syrups, suppositories, and lollipops.[7]
- Codeine (Various brand names; often combined with acetaminophen and aspirin)
- Fentanyl (Actiq®, Duragesic®, Fentora®)
- Hydrocodone (Hysingla ER®, Zohydro ER®, Lortab®, Norco®, Vicodin®)
- Hydromorphone (Dilaudid®, Exalgo®)
- Meperidine (Demerol®)
- Methadone (Dolophine®, Methadose®)
- Morphine (Avinza®, Kadian®, MS Contin®, Ora-Morph SR®)
- Oxycodone (OxyContin®, Roxicodone®, Percocet®, Targiniq ER®)
- Oxymorphone (Opana®)


ACUTE VS. CHRONIC PAIN
The patient population in the workers’ compensation industry is often managed with opioid therapy to treat pain linked to a work-related injury. The use of opioids to treat pain, however, can lead to negative outcomes and adverse events, such as addiction. According to the International Association for the Study of Pain (IASP), pain is an unpleasant sensory and emotional experience associated with actual or potential tissue damage, or described in terms of such damage and can be further classified as acute or chronic.[8]
Acute pain most commonly occurs after surgery or immediately after an injury. Typically, acute pain becomes increasingly manageable as the body heals and usually lasts less than three months. In comparison, chronic pain persists for more than three months and can be the result of numerous causes. In the workers’ compensation industry, chronic pain can be especially devastating, as it negatively affects not only the claimant’s well-being, but also the path to recovery. In fact, approximately 32 percent of work-related injuries are being treated with opioids in the United States. The costs for claims linked to a diagnosis of chronic pain are substantial for employers due to prescription medication, treatments and/or a delayed return to work. A recent study published in the Journal of the American Medical Association found that the use of an opioid pain medication in managing chronic pain was no more effective than a non-opioid alternative, such as ibuprofen and acetaminophen.[9]
OPIOID PRESCRIBING GUIDELINES
Insurance companies and third-party administrators should utilize best practices to help injured workers with chronic pain by working with medical providers to prevent opioid addiction and abuse.
The government is taking several steps in attempting to control the growing issue of prescription opioid abuse. In an effort to reduce the rate at which these high-risk drugs are prescribed and to educate patients on the potential risks, the U.S. Food and Drug Administration (FDA) issued a statement effective March 2016 that strong prescription opioid painkillers will be required to carry a “black box” warning regarding the high risk of abuse, addiction, overdose, and death.[10]
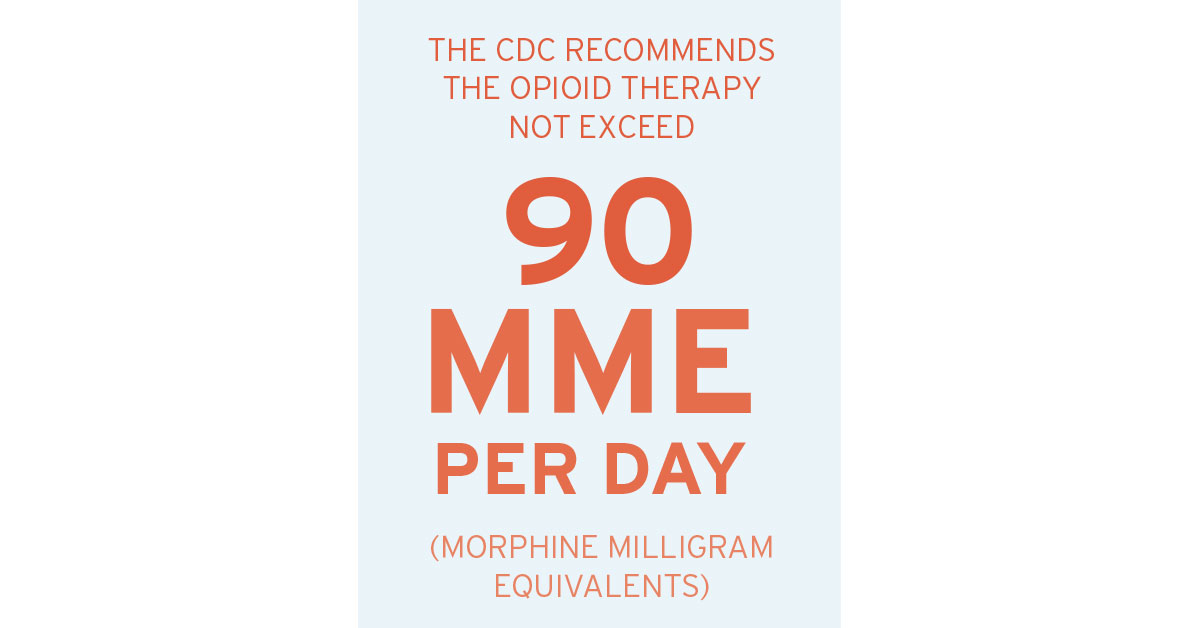
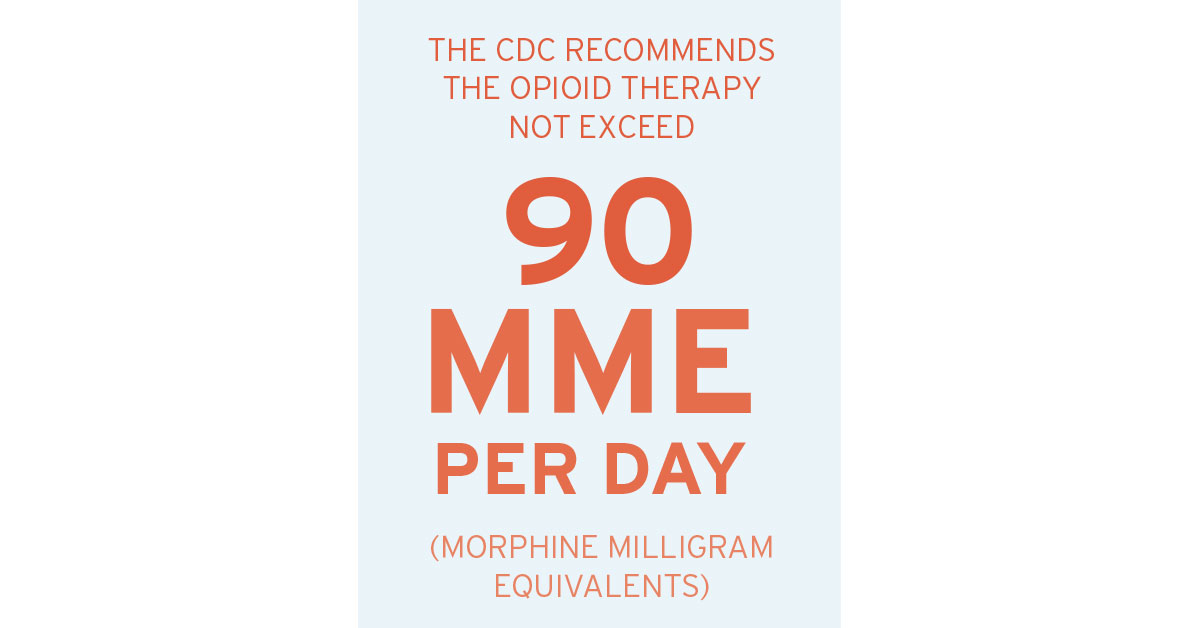
In addition, the CDC published the “CDC Guideline for Prescribing Opioids for Chronic Pain” to provide recommendations on prescribing opioids for chronic pain outside of active cancer treatment, palliative care, and/or end-of-life care. By focusing on improving communication between providers and patients about the risks and benefits of opioid therapy for chronic pain, these guidelines seek to improve the safety and effectiveness of the treatment of pain and reduce the risks linked to opioid therapy for chronic pain, including opioid use disorder and overdose. It also suggests non-opioid alternative therapies as the first-line of treatment along with regulated use of opioid analgesic—usually less than seven days of initial therapy for most acute injuries. The CDC recommends the opioid therapy not exceed 90 Morphine Milligram Equivalents (MME) per day. A determination to titrate above 90 MME to achieve the anticipated clinical effect.5 Utilizing consistent, unplanned urine drug screenings and
reviewing prescription drug monitoring programs (PDMP) to aid in managing the opioid therapy is also encouraged.[10] Throughout the United States, related statebased guidelines are in effect, under review and/or are in development. Completely understanding the different gradations of the new requirements for each state gives adjusters, claimants, and physicians the instruments needed to better manage the utilization of opioid therapy and the treatment of chronic pain.
Insurance companies and third-party administrators should utilize best practices to help injured workers with chronic pain by working with medical providers to prevent opioid addiction and abuse. They can do so by focusing on evidencebased alternative therapy treatments for chronic pain. This can be accomplished by utilizing PBM services that defer to approved formularies, point-ofsale, and retrospective strategies. In the workers’ compensation industry, the risks associated with opioids should be addressed by providers and claim managers by utilizing programs that require the moderate use of opioid medication for manageable pain. The ultimate goal is a reduction of pain, clinical improvement of function, and prevention of opioid dependency for the injured worker. Claims professionals need to develop a strategic plan for identifying potential opioid abuse by monitoring physician prescribing patterns and the specific use patterns for each claim.
The overall strategy in managing claims involving opioids can benefit the employer and the injured worker by implementing the following best practices:
- Performing pharmacy utilization reviews
- Monitoring physician dispensing and prescribing patterns
- Utilizing nurse case management, early intervention, and consistent monitoring
- Implementing prescription drug card programs
- Utilizing physicians that use state prescription drug monitoring programs and tools
- Investigating resources to discover behavioral patterns that suggest the potential for abuse
- Evaluating the cost of opioids compared to alternatives


MANAGING CHRONIC PAIN IN INJURED WORKERS
Opioid utilization must be managed and monitored by physicians, pharmacies, and pharmacy benefit management companies. Effective management provides claimant safety, improved health, a more sustainable approach to pain relief, and a potential earlier return to work. Furthermore, managing opioids reduces costs and alleviates risk for the employer.
EARLY INTERVENTION
A best practice in combating opioid abuse is ensuring appropriate treatment for the injured worker from the very beginning. Early intervention establishes firm parameters from the inception of the claim. Proactive claim management practices should be present during the initial provider appointment and the point-of-sale when the injured worker fills the first prescription.
COMPLIANCE
In order to best serve its claimants and clients, a PBM should proactively ensure that it remains compliant with state and federal laws regarding opioid prescription medications. As states look to curb the opioid crisis by restricting the initial days’ supply of opioid medication, PBMs must also have resources and guidelines in place for complying with these new regulations as they are passed into law. A PBM should also make insurance adjusters aware when a claimant receives medications that deviate from a state-regulated formulary or the Official Disability Guidelines (ODG) formulary. Contacting the insurance adjuster will help increase their awareness regarding formulary regulation and potentially reduce the number of medications that do not relate to the claimant’s injury.
LETTER OF MEDICAL NECESSITY
A Letter of Medical Necessity (LMN) is a valuable tool used by PBMs to help manage opioid claims. A PBM can identify claimants with an opioid prescription history outside of the CDC guidelines and can request an LMN be completed by the claimant’s Authorized Treating Physician (ATP). If no response is given regarding the necessity of a medication, a PBM may choose to temporarily restrict access to a medication at the point-of-sale, providing a real-time intervention until the necessity of a medication can be determined. This real-time intervention also serves as an opportunity to educate the claimant regarding the risks associated with opioid use in the long-term. In the event contact with the ATP cannot be established via a LMN, a nurse case manager should be used to contact the ATP to discuss the plan of care and any alternative treatment options that may be available.


MONITORING AND MANAGING
Another important step for claim managers is monitoring and managing opioid abuse. By identifying claimants struggling with an opioid addiction—a problem they never intended to have—claim managers and their partners can provide support for reducing opioid dependency. Supplementing the reduction or restriction of opioids by other measures to help the injured worker recover, manage the pain productively, and return to work is the ultimate goal. When identified, the nurse case manager should follow-up with the physician regarding prescribing patterns that do not follow the opioid prescribing guidelines. (It can also be beneficial for employers if the PBM and the TPA provide a notification to them when they identify an opioid prescription has been dispensed.)
NURSE CASE MANAGERS
In claims that involve pain management, nurse case managers can help injured workers recover from and/or avoid opioid dependence. Nurse case managers are particularly situated as the liaison between all parties involved in caring for the injured worker. Nurse case managers are educated on appropriate opioid drug therapy and duration. They are able to discuss alternatives for pain management with physicians and educate patients about the risks and short-term benefits of opioids. They can identify risk factors like previous alcohol or drug dependence. They can also make the physician aware of co-morbidities, such as sleep apnea or mental health conditions, whereby risks may outweigh the benefits of opioids. Nurse case managers help create a safer environment for claimants with chronic pain by encouraging physicians to consider other treatment options and raising awareness of opioid abuse. They can assist physicians in developing a treatment plan that includes a safe opioid weaning schedule prepared in collaboration with a pharmacist and the transition toward alternative therapies. Nurse case managers can intervene from the start and work with physicians to develop a pain management plan tailored to the injured worker’s needs. If the treating physician prescribes opioids, goals and benchmarks are established at the beginning of the treatment plan. In addition, goal setting is especially important prior to surgery to help establish realistic expectations and educate the physician and claimant about post-operative pain management.
DRUG UTILIZATION REVIEWS
When monitoring claims and intervening on the patient’s behalf prove to be unsuccessful, a Drug Utilization Review (DUR) should be considered. DURs provide the building blocks necessary to determine the medical necessity and appropriateness of the treatment rendered.
DURs allow for the review of an injured worker’s treatment records to determine the medical necessity of the medications as related to the work injury. The pharmacist and physician performing the DUR are trained to determine if a prescribed medication is safe, appropriate, and necessary to treat the injury. They can determine cost-effective alternatives that aid in returning the claimant to good health and restoring productivity. Pharmacists and PBMs understand the importance of value-based care and how appropriate treatments can be provided while eliminating unnecessary costs for the employer.
- Limits on first fill of dispensed opioids
- Step therapy
- Educating injured workers with material about dangers of opioid use with the first fill
- Requesting LMNs from the physician
- Promoting home delivery pharmacy service for additional opioid oversight
- Monitoring state reporting on controlled substances
- Compliance with state guidelines pertaining to opioid management (Example: New York, Tennessee, Texas, Oklahoma, Kentucky, and New Jersey)
- Opioid Case Management Prescription Reviews
- Consulting with the physician to provide alternative therapy for long-term opioid patients
CASE MANAGEMENT PRESCRIPTION REVIEW PROGRAM
Carlisle Medical’s Case Management Prescription Review is a comprehensive clinical review performed by a Carlisle staff pharmacist and registered nurse with the goal of achieving maximum savings by providing cost-effective drug therapy recommendations. Case Management Prescription Reviews have shown to be effective in reducing future medication expenses. This program will continue to be a valuable cost-savings tool as the price of an opioid claim has increased from $460 in 2012 to $574 in 2016 and has shown no signs of slowing down.[11]
KEY INDICATORS FOR PRESCRIPTION REVIEW
- Opioid usage outside the CDC Guidelines
- Claimant’s monthly medication cost exceeds $500
- Claim is approaching settlement/Medicare Set-Aside
- Claimant is prescribed brand medications that have a generic equivalent
- Claimant is prescribed two or more medications in the same therapeutic class
- Multiple prescribing physicians
CASE STUDIES
CASE STUDY ONE: Abstral®
A claimant was receiving a brand name medication Abstral®, which is a sublingual form of fentanyl. Per the FDA guidelines, this medication is only approved for breakthrough cancer pain in opioid-tolerant patients. In this case, the claimant was being treated for pain following a lumbar fusion procedure. The sedating properties of Abstral® were so profound that the ATP also prescribed Modafinal®, which is only FDA-approved for sleep disorders, such as narcolepsy and sleep apnea. Highly medicated and in pain, the claimant’s quality of life was suffering as a result of the prescribed medications and the physician’s disregard for prescribing guidelines.
Carlisle Medical’s Case Management Prescription Review presented the physician with alternatives to Abstral®, which would not only decrease the amount of narcotic medication, but would also eliminate the need for a psychostimulant like Modafinil®. Also, the pharmacist noted that the stimulating properties of Modafinal® had been counteracting the pain relieving properties of Abstral®. The nurse presented these alarming findings to the ATP, who then agreed to stop the sublingual Abstral® in exchange for an alternative pain medication that provided the claimant with a more appropriate pain reliever at a lower cost and with less risk of addiction. The Case Management Prescription Review provided a direct benefit to the claimant’s quality of life and reduced the medication costs associated with the claim.
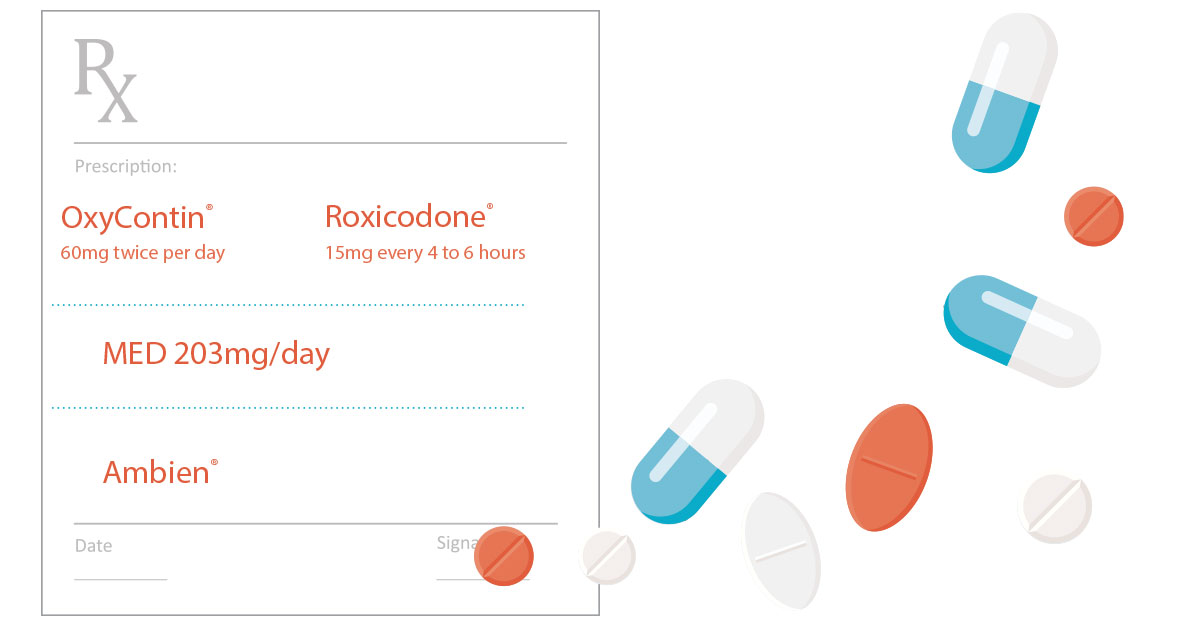
CASE STUDY TWO: OxyContin®
A claimant was prescribed OxyContin® extended relief 60mg twice per day and Roxicodone® immediate release 15mg every four to six hours. The total morphineequivalent dose (MED) of both opioids was 203mg/day. The claimant was also prescribed Ambien® for sleep deprivation. The presence of potent opioids coupled with sleep medication identified this claimant as being at a higher risk for opioid abuse and in need of assistance to improve the quality of life.
A DUR was performed and the findings were sent to the ATP. After two months passed with no response, Carlisle Medical was asked to have a nurse case manager present the findings directly to the
physician. During a consultation with the physician, he agreed to safely titrate down the total MED to 100mg/day. The nurse case manager also was able to educate the claimant on the risks associated with opioids and sleep aids, which are both Central Nervous System (CNS) depressants.
CONCLUSION
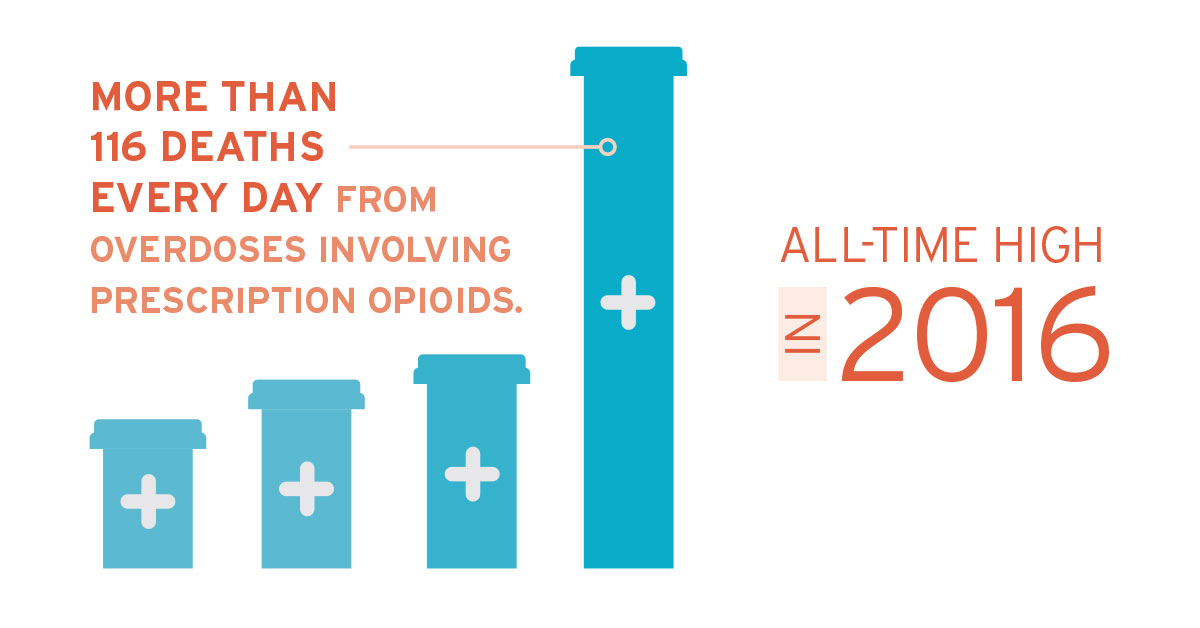
The use of opioid analgesics has been under scrutiny by stakeholders throughout the system due to the growing number of overdoses and deaths related to opioid abuse. In the workers’ compensation industry, claimants are commonly prescribed opioid therapy to treat pain associated with an injury. Despite serious risks and lack of evidence regarding their longterm effects, the United States has seen a significant rise in the acceptance and use of prescription opioids for the treatment of chronic pain. In 2016, the opioid related death toll reached an all-time high—showing more than 116 deaths every day from overdoses involving prescription opioids.[12]
Although there is a place for opioid therapy in the pain management of injured workers, the United States has reached epidemic proportions of abuse in many states. This rising epidemic has led to a broad assortment of responses from a variety of stakeholders, including numerous states that are forming their own strategies to fight back.
State and federal governments are strengthening their efforts on initiatives to stem the tide of the damage caused by opioids. A surge of state implemented laws limiting the duration and dosage of initial opioid prescriptions has been passed. Because of these efforts, the prescribing rates and morphine-equivalent dose (MED) levels are finally on a downward trend nationwide.
In all circumstances, the primary goal is to ensure opioid therapy is the appropriate treatment for the injured worker, the medication is prescribed at the appropriate time and in the proper dose, and is prescribed for the applicable duration with ongoing management and monitoring to ensure clinical safety and efficacy of care. As with most medication therapy regimens, using the lowest possible dose for the shortest duration of time is a best practice in opioid therapy management. The use of non-medication therapy, including physical or occupational therapy, may also be an appropriate first-line therapy approach to acute injuries. Furthermore, the benefits of therapy must outweigh the risks. Care must be taken to confirm opioid medications are right for the claimant and their injury, as well as prescribed in the right dose and for the right duration.
In claims involving pain management, nurse case managers are an essential part of helping injured workers recover and avoid opioid dependence. Because of their clinical backgrounds, nurse case managers play an invaluable role working with physicians. They can help injured workers reduce opioid use by collaborating with physicians and pharmacists to monitor prescriptions from all prescribers.
Slowing the nation’s opioid crisis takes a collaborative effort by all parties involved throughout the claim life cycle. Data mining to identify claimants at risk, nurse case management, and PBM services are vital factors to a program’s success.


ADDITIONAL RESOURCES
This white paper was prepared by Carlisle Medical. Carlisle Medical has more than 38 years of experience as a leader in containing health care costs in the workers’ compensation industry. Our company can help insurance carriers, third-party administrators, and employers significantly reduce their workers’ compensation costs. Our experienced staff of licensed pharmacists and nurses can assist companies with injuries, ranging from minor to catastrophic.
INTERNAL EDUCATION
Educating claimants about costly and addictive treatment can be helpful. Behavioral research has demonstrated that claimants care about the costs of the treatments they receive, including physician-dispensed medication. Employers can further alleviate the rising drug costs associated with opioid analgesics by educating adjusters, case managers, and risk management resources personnel on Case Management Prescription Review services.
REFERENCES:
[1] IIHS. (2018). General statistics. [online] Available at: http://www.iihs.org/iihs/topics/t/general-statistics/fatalityfacts/overview-offatality-
facts/2016
[2] ODG, Chronic Pain, 2016 Chronic, Undertreated Pain Affects 116 Million Americans. Szalavitz, M., Time, June 29, 2011
[3] Goetz, T. (2018, March 22). The Most Popular Drugs in America, State by State. Retrieved March 23, 2018, from https://www.goodrx.com/blog/the-most-popular-drugs-in-america-by-state/?utm_source=newsletter&utm_medium=email&utm_campaign=newsletter_axiosvitals&stream=top-stories
[4] Hedegaard H, Warner M, Miniño AM. Drug overdose deaths in the United States, 1999–2016. NCHS Data Brief, no 294. Hyattsville, MD: National Center for Health Statistics. 2017/ CDC. Wide-ranging online data for epidemiologic research (WONDER). Atlanta, GA: CDC, National Center for Health Statistics; 2016. Available at http://wonder.cdc.gov
[5] Media Relations. “Opioid Prescribing Is Still High and Varies Widely throughout the U.S.” Center for Disease Control and Prevention, CDC, 6 July 2017, 1:00pm, www.cdc.gov/media/releases/2017/p0706-opioid.html.
[6] Office of the Press Secretary, February 02, 2016, FACT SHEET: President Obama Proposes $1.1 Billion in New Funding to Address the Prescription Opioid Abuse and Heroin Use Epidemic
[7] DEA. “Drug Facts Sheets – Narcotics.” Drug Enforcement Administration, www.dea.gov/druginfo/factsheets.shtml.
[8] International Association for the Study of Pain. “Pain.” IASP Taxonomy – IASP, www.iasppain.org/Taxonomy.
[9] Krebs EE, Gravely A, Nugent S, Jensen AC, DeRonne B, Goldsmith ES, Kroenke K, Bair MJ, Noorbaloochi S. Effect of Opioid vs Non-opioid Medications on Pain-Related Function in Patients With Chronic Back Pain or Hip or Knee Osteoarthritis Pain The SPACE Randomized Clinical Trial. JAMA. 2018; 319 (9): 872–882. doi:10.1001/jama.2018.0899
[10] Center for Drug Evaluation and Research. “Drug Safety and Availability – FDA Drug Safety Communication: FDA Warns about Serious Risks and Death When Combining Opioid Pain or Cough Medicines with Benzodiazepines; Requires Its Strongest Warning.” U S Food and Drug Administration Home Page, Center for Drug Evaluation and Research, www.fda.gov/Drugs/DrugSafety/ ucm518473.html.
[11] National Council on Compensation Insurance Inc. (NCCI), NCCI Medical Data Report: Opioid Utilization Supplement for the State of: Montana, September 2016, pdf.
[12] CDC.gov. (2017). Drug Overdose Death Data | Drug Overdose | CDC Injury